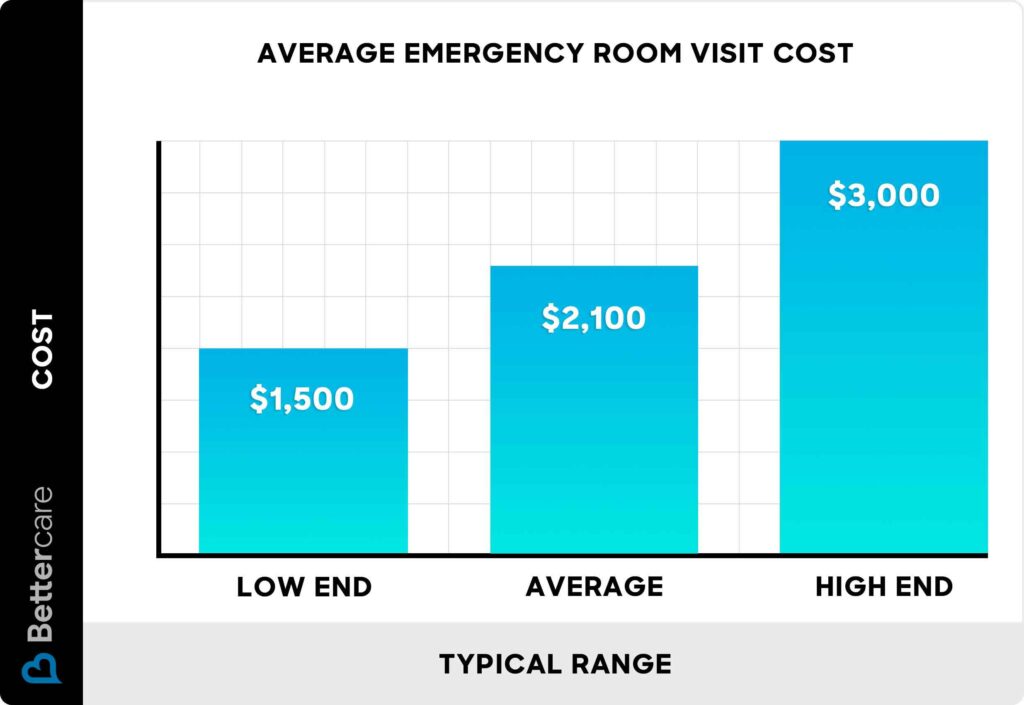
Navigating the healthcare system can be complex, and emergency room (ER) visits often come with unexpected costs. Many people wonder if do emergency rooms charge by the hour, leading to anxiety about potential financial burdens. This article aims to demystify ER billing practices, providing a comprehensive understanding of how ERs calculate charges and what factors influence those costs. We’ll explore common ER charges, tips for understanding your bill, and available payment options to help you navigate this process with confidence.
Emergency Room Billing Explained
Do emergency rooms charge by the hour? The short answer is no. ERs do not operate on an hourly billing system. Instead, they bill based on the specific medical services provided during your visit. This means that the cost of your ER visit will depend on the nature and complexity of your condition, the treatments required, and any procedures performed.
ER billing typically involves a combination of charges for:
* Emergency room evaluation: This fee covers the physician’s initial assessment and examination.
* Diagnostic tests: Blood work, X-rays, CT scans, and other diagnostic tests ordered by the physician will incur separate charges.
* Medications: Any medications administered during your ER visit, including pain relievers, antibiotics, or intravenous fluids, will be billed separately.
* Treatments: Procedures such as wound care, splinting, or IV insertion will also have associated costs.
Factors Affecting ER Costs

Several factors can influence the overall cost of an ER visit.
Severity of Condition:
The complexity and severity of your medical issue play a significant role in determining the charges. A minor injury requiring basic treatment will generally cost less than a life-threatening emergency necessitating extensive procedures and prolonged hospitalization.
Location and Type of Facility:
ERs located in urban areas or specialized hospitals often have higher costs compared to rural facilities. The type of hospital, whether it’s a public or private institution, can also affect pricing.
Insurance Coverage:
Your health insurance plan significantly impacts your out-of-pocket expenses. Different plans have varying levels of coverage for ER visits, deductibles, and copayments.
Common ER Charges
While specific charges vary widely based on location and services rendered, here are some common categories and estimated costs:
- Emergency room evaluation: $200 – $500
- Diagnostic tests (X-ray): $100 – $300
- Blood work: $50 – $150
- Medications: Varies depending on the type and dosage.
- Treatments (wound care, splinting): $50 – $200
Understanding Your ER Bill

Receiving your ER bill can be overwhelming. Take time to carefully review each line item and understand what it represents.
- Itemized list: Look for a detailed breakdown of all charges, including procedures, medications, and supplies.
- CPT codes: These five-digit codes identify specific medical services performed. You can use online resources to find descriptions of these codes.
- HCPCS codes: These codes represent supplies and equipment used during your visit.
Payment Options for ER Bills
If you’re facing a significant ER bill, explore available payment options:
- Insurance coverage: Contact your insurance provider to understand your benefits and potential out-of-pocket expenses.
- Payment plans: Many hospitals offer flexible payment plans to spread out the cost over time.
- Financial assistance programs: Some hospitals have financial assistance programs for patients with limited income.
Conclusion
Understanding how ERs bill can help you navigate this process with greater confidence. Remember that ERs do not charge by the hour but rather base their fees on the specific services provided. By carefully reviewing your bill, exploring payment options, and communicating with your insurance provider, you can effectively manage the financial aspects of an ER visit.