Navigating the world of mental health care can feel overwhelming, especially when you’re unsure about the necessary steps. One common question is whether you need a referral to see a therapist. The answer isn’t always straightforward and depends on several factors, primarily your insurance plan and the laws in your state. Understanding these nuances can empower you to seek the support you need without unnecessary hurdles.
This article will delve into the complexities of therapy referrals, exploring how insurance coverage and state regulations influence your access to mental health professionals. We’ll also discuss the importance of in-network therapists and provide clear guidance on contacting your insurance company for specific information about your plan.
Therapy Referrals
A referral is essentially a recommendation from one healthcare professional to another, authorizing you to receive specialized care. In the context of therapy, this often means a primary care physician (PCP) recommending you to a mental health specialist like a psychologist, psychiatrist, or licensed clinical social worker. While referrals can be helpful in ensuring coordinated care, they aren’t always mandatory.
The need for a referral varies significantly depending on your insurance plan and state regulations. Some insurance companies require a referral from your PCP before covering therapy sessions, while others offer direct access to mental health professionals. This means you might be able to schedule an appointment with a therapist directly without needing prior authorization from your PCP.
It’s important to remember that even if your insurance doesn’t technically require a referral, your PCP can still play a valuable role in your mental health journey. They can provide initial assessments, rule out any underlying medical conditions contributing to your emotional well-being, and offer guidance on finding appropriate therapists.
Insurance Coverage

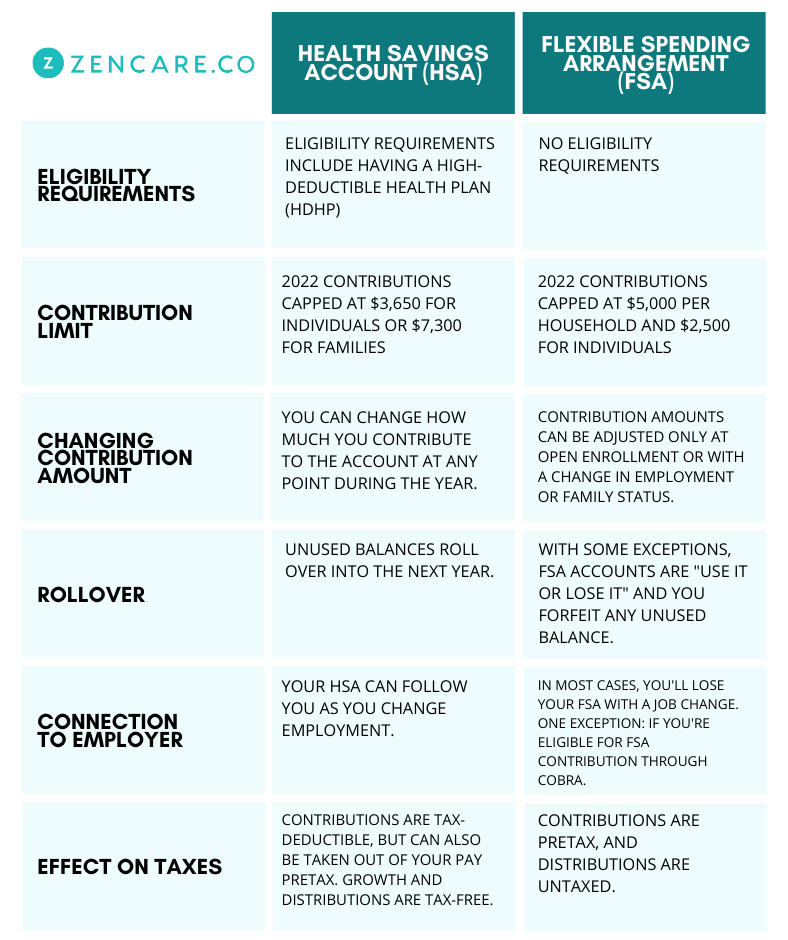
Your insurance plan plays a crucial role in determining whether you need a referral for therapy and what level of coverage you receive. Different plans have varying policies regarding mental health benefits, including requirements for referrals, copayments, and the number of sessions covered per year.
To understand your specific coverage, carefully review your insurance policy documents or contact your insurance provider directly. Pay attention to terms like “mental health parity,” which ensures that your mental health benefits are comparable to your physical health benefits. Additionally, inquire about any limitations on the types of therapists covered (e.g., psychologists vs. psychiatrists) and whether there are specific diagnoses that require pre-authorization.
State Laws
State laws also influence access to mental health care, including referral requirements. Some states have implemented “parity laws” that mandate insurance companies to provide equal coverage for mental health and physical health services. These laws can vary in their scope and enforceability, so it’s essential to research the specific regulations in your state.
Additionally, some states have established licensing boards for mental health professionals that may set guidelines regarding referrals or direct access to therapy. For example, certain states allow licensed therapists to practice independently without requiring a referral from a PCP.
In-Network Therapists

Choosing an in-network therapist can significantly impact your out-of-pocket expenses. In-network providers have negotiated rates with your insurance company, meaning you’ll typically pay lower copayments or deductibles for their services.
When searching for a therapist, always verify their status within your insurance network. You can usually find this information on your insurance company’s website or by calling their customer service line. Remember that even if a therapist is in-network, it’s crucial to confirm their specific specialties and treatment approaches to ensure they align with your needs.
Contact Your Insurance Company
The most reliable way to determine whether you need a referral for therapy is to contact your insurance company directly. They can provide detailed information about your plan’s specific requirements, including any referral policies, coverage limits, and in-network therapists in your area.
Conclusion
Understanding the complexities of therapy referrals requires careful consideration of your insurance plan and state regulations. While some insurance companies require referrals from primary care physicians, others offer direct access to mental health professionals. By contacting your insurance company directly and exploring in-network therapists, you can navigate this process effectively and prioritize your mental well-being. Remember that seeking professional support is a sign of strength, and taking these steps can empower you to embark on a journey towards improved mental health.